Mucoepidermoid Carcinoma (MEC) & Warthin-like MEC
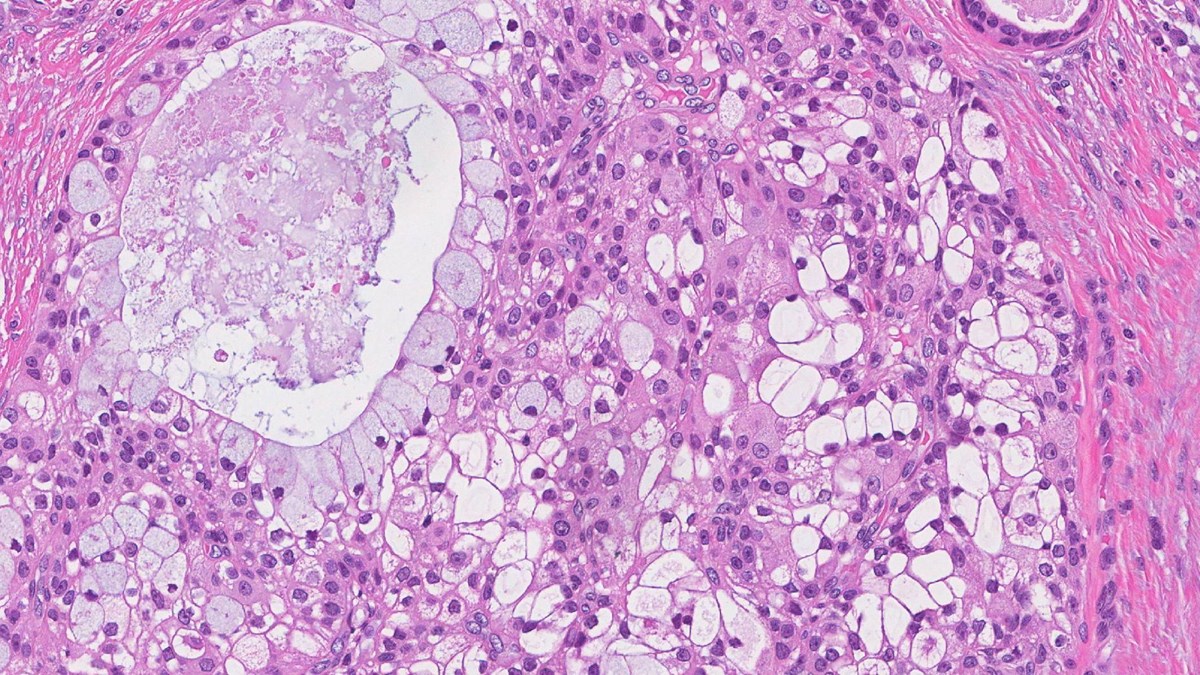
Mucoepidermoid carcinoma (MEC)
Mucoepidermoid carcinoma (MEC) is the most common salivary gland cancer in adults and children (1, 2). The cancer affects more women than men and is most likely to develop in the 40s or 50s (2, 3). The major salivary glands are responsible for producing approximately 95% of saliva and include the parotid (just below and in front of each ear), the submandibular (below the jaws) and the sublingual glands (under the tongue) (4). Minor salivary glands produce the remaining saliva and can be found in almost any part of the mouth (4). Most MEC forms in the parotid gland, although they can also develop in the submandibular and minor salivary glands (2). MEC have been reported at distant sites including the breast, lungs, and thyroid (5-6). MEC typically form a slow-growing, painless lump below the ears, and common symptoms include weakness or twitching in the face, pain or tenderness, ear discharge, trouble swallowing and difficulty opening the mouth (8-10).
Ultrasound is used to guide a fine needle into the parotid or submandibular gland to collect a small sample of cells, which will then be examined under the microscope. Genetic analysis of MEC has revealed an unusual rearrangement of chromosomes, producing a fusion of MECT1 and MAML2 genes (11). This rearrangement is found in less aggressive types of MEC and is often associated with a better long-term outcome.
Less aggressive MEC is slow growing, whereas aggressive forms of MEC are fast growing and characterised by cells that spread into surrounding parts of the body, including lymph nodes (1). Less aggressive MEC, particularly those with MECT1-MAML2 gene fusion, have a good long-term outcome, with 90% of patients living 5-years after surgery (2). Aggressive MEC have much poorer long-term outlook as they have a high chance of returning, and often spread to other tissues (12).
The main treatment is surgery to remove the entire cancer, with healthy tissue around it. The challenge is to remove enough tissue without causing damage to the nearby facial nerve (10). Radiotherapy is recommended after surgery for patients with aggressive forms of MEC, and if the entire cancer is unable to be removed by surgery (13). There have also been several clinical trials that have researched different ways to treat MEC (13). Clinical trials have investigated chemotherapies (cisplatin, paclitaxel, and docetaxel), monoclonal antibody (trastuzumab), and targeted therapies (sorenafib, nintedanib, lapatinib, and vorinostat) which exploit differences between cancer cells and normal cells (10, 13).
In April 2024, Nature published a paper 'Machine learning-based survival prediction nomogram for postoperative parotid mucoepidermoid carcinoma' and you can access it here.
Warthin-like mucoepidermoid carcinoma (Warthin-like MEC)
Warthin-like mucoepidermoid carcinoma (Warthin-like MEC) is a very rare type of salivary gland cancer that has only recently been identified (14). Warthin tumour is a harmless lump in the salivary gland, which has unique features. The term Warthin-like MEC was given to describe mucoepidermoid carcinoma with features of Warthin tumour (14). There have been very few cases of Warthin-like MEC reported, which makes it difficult to understand who it is most likely to affect (15). All cases of Warthin-like MEC that have been reported have occurred in the parotid gland (just below and in front of each ear) and usually form a painless lump (15).
As Warthin-like MEC is so rare and there are many differences between each reported case, it is very difficult to diagnose. Genetic analysis of Warthin-like MEC has revealed an unusual rearrangement of the MALM2 gene, which can be used to diagnose the cancer alongside examination of cells under the microscope (15).
Warthin-like MEC is often described as a less aggressive tumour and the long-term outlook is good, particularly for tumours containing the MALM2 gene rearrangement (14). The main treatment is surgery, and in some cases surrounding lymph nodes are removed. Radiotherapy and radioactive iodine treatment may also be offered (15). It is unlikely that the tumour will return following surgery (15).
Useful resources
Read more about how to get your tumour profiled and add to the research biobank at the Christie Hospital in Manchester, UK here:
- Gene profiling or tumour profiling or genomic testing - Salivary Gland Cancer UK
- Donate tissue to the Biobank - Salivary Gland Cancer UK
References
1. Nance MA, Seethala RR, Wang Y, Chiosea SI, Myers EN, Johnson JT, Lai SY. Treatment and survival outcomes based on histologic grading in patients with head and neck mucoepidermoid carcinoma. Cancer. 2008;113(8):2082-9.
2. Young A, Okuyemi OT. Malignant Salivary Gland Tumors. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024.
3. Boukheris H, Curtis RE, Land CE, Dores GM. Incidence of carcinoma of the major salivary glands according to the WHO classification, 1992 to 2006: a population-based study in the United States. Cancer Epidemiol Biomarkers Prev. 2009;18(11):2899-906.
4. Ghannam M, Singh P. Anatomy, Head and Neck, Salivary Glands Treasure Island (FL): StatPearls Publishing; [updated 2023 May 29. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538325/.
5. Hastrup N, Sehested M. High-grade mucoepidermoid carcinoma of the breast. Histopathology. 1985;9(8):887-92.
6. Green LK, Gallion TL, Gyorkey F. Peripheral mucoepidermoid tumour of the lung. Thorax. 1991;46(1):65-6.
7. Wenig BM, Adair CF, Heffess CS. Primary mucoepidermoid carcinoma of the thyroid gland: a report of six cases and a review of the literature of a follicular epithelial-derived tumor. Hum Pathol. 1995;26(10):1099-108.
8. Sharma S, Khan S, Valiathan M. Mucoepidermoid carcinoma - A common neoplasm at an unusual site, mimicking a benign cyst on cytology: Diagnostic pitfall! J Oral Maxillofac Pathol. 2022;26(Suppl 1):S30-s3.
9. Boahene DKO, Olsen KD, Lewis JE, Pinheiro AD, Pankratz VS, Bagniewski SM. Mucoepidermoid Carcinoma of the Parotid Gland: The Mayo Clinic Experience. Archives of Otolaryngology–Head & Neck Surgery. 2004;130(7):849-56.
10. van Herpen C, Vander Poorten V, Skalova A, Terhaard C, Maroldi R, van Engen A, et al. Salivary gland cancer: ESMO-European Reference Network on Rare Adult Solid Cancers (EURACAN) Clinical Practice Guideline for diagnosis, treatment and follow-up. ESMO Open. 2022;7(6):100602.
11. Yin LX, Ha PK. Genetic alterations in salivary gland cancers. Cancer. 2016;122(12):1822-31.
12. Nishimura H, Jin D, Kinoshita I, Taniuchi M, Higashino M, Terada T, et al. Increased Chymase-Positive Mast Cells in High-Grade Mucoepidermoid Carcinoma of the Parotid Gland. Int J Mol Sci. 2023;24(9).
13. Sama S, Komiya T, Guddati AK. Advances in the Treatment of Mucoepidermoid Carcinoma. World J Oncol. 2022;13(1):1-7.
14. Yan L, Xu J, Liu L, Li X. Warthin-like mucoepidermoid carcinoma of the parotid gland: Clinicopathological observation and literature review. Sci Prog. 2023;106(2):368504231179816.
15. Wang X, Liu L, He H, Li B. MAML2 gene rearrangement occurs in all Warthin-like mucoepidermoid carcinoma: A reappraisal in a series of 29 cases. Heliyon. 2024;10(2):e24873.
Last updated April 2024
'Machine learning-based survival prediction nomogram for postoperative parotid mucopidermoid carcinoma' Abstract
Parotid mucoepidermoid carcinoma (P-MEC) is a significant histopathological subtype of salivary gland cancer with inherent heterogeneity and complexity. Existing clinical models inadequately offer personalized treatment options for patients. In response, we assessed the efficacy of four machine learning algorithms vis-à-vis traditional analysis in forecasting the overall survival (OS) of P-MEC patients. Using the SEER database, we analyzed data from 882 postoperative P-MEC patients (stages I–IVA). Single-factor Cox regression and four machine learning techniques (random forest, LASSO, XGBoost, best subset regression) were employed for variable selection. The optimal model was derived via stepwise backward regression, Akaike Information Criterion (AIC), and Area Under the Curve (AUC). Bootstrap resampling facilitated internal validation, while prediction accuracy was gauged through C-index, time-dependent ROC curve, and calibration curve. The model’s clinical relevance was ascertained using decision curve analysis (DCA). The study found 3-, 5-, and 10-year OS rates of 0.887, 0.841, and 0.753, respectively. XGBoost, BSR, and LASSO stood out in predictive efficacy, identifying seven key prognostic factors including age, pathological grade, T stage, N stage, radiation therapy, chemotherapy, and marital status. A subsequent nomogram revealed a C-index of 0.8499 (3-year), 0.8557 (5-year), and 0.8375 (10-year) and AUC values of 0.8670, 0.8879, and 0.8767, respectively. The model also highlighted the clinical significance of postoperative radiotherapy across varying risk levels. Our prognostic model, grounded in machine learning, surpasses traditional models in prediction and offer superior visualization of variable importance.