Adenocarcinoma
Adenocarcinoma
Polymorphous adenocarcinoma (PAC)
PAC is a salivary gland cancer found mostly in women across a wide range of ages, with most cases occurring at around 60 years of age (1). The cancer forms in the minor salivary glands of the mouth or throat, specifically in the roof of the mouth, and doesn't cause any symptoms (2). Minor salivary glands produce 5% to 8% of saliva and can be found in almost any part of the mouth (3).
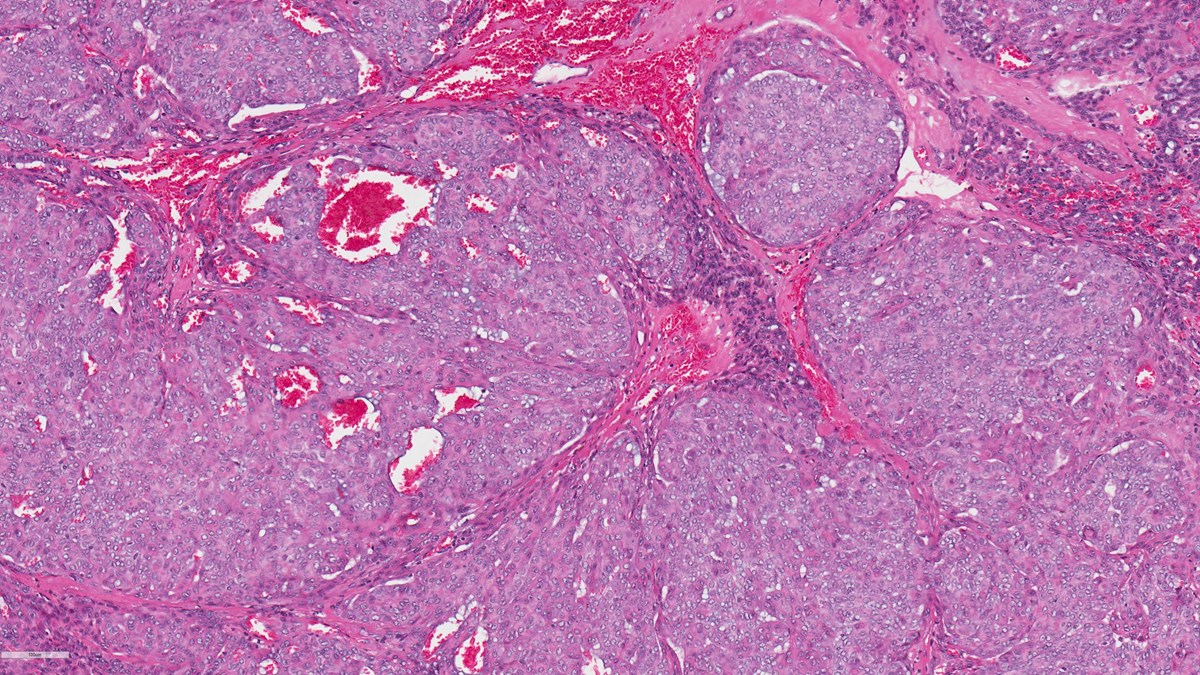
Experts can diagnose PAC by looking at cells under a microscope. The cancer cells themselves look the same, but they clump together in different ways, and they often spread to nearby tissues (1). Most PAC cases have a specific genetic mutation known as PRKD1 E710D which can help with diagnosis (4, 5).
PAC is usually a slow growing, non-aggressive tumour, which rarely spreads to other parts of the body and has a good chance of successful treatment (1, 5). The main treatment is surgery to remove the tumour, including the underlying bone, if necessary. Surgery is normally followed by radiotherapy (2).
Cribriform adenocarcinoma of salivary glands (CASG)
CASG has been found in both major salivary glands and minor salivary glands. The major salivary glands are responsible for producing approximately 95% of saliva and include the parotid (just below and in front of each ear), the submandibular (below the jaws) and the sublingual glands (under the tongue) (3). Minor salivary glands produce the remaining saliva and can be found in almost any part of the mouth (3). Most cases of CASG are found in the tongue (5, 6).
CASG are characterised by small cysts and lumps, and when examined under the microscope the tumour appears to contain holes (5). Most CASG have been shown to have genetic abnormalities, such as fusions or rearrangements of the PRKD1, PRKD2 and PRKD3 genes (6, 7).
CASG is aggressive and has a high chance of spreading to the lymph nodes (8). The main treatment is surgery followed by radiotherapy and in some cases lymph nodes in the neck may have to be removed if the cancer has spread (7, 8).
Mucinous adenocarcinoma (MAC)
MAC is an extremely rare salivary gland cancer, affecting mostly men in their 50s and 60s (6, 9, 10). MAC typically occurs in minor salivary glands, which produce 5% to 8% of saliva and can be found in almost any part of the mouth (3).
Most MAC is found in the roof of the mouth (palate), and usually does not cause any symptoms (10). There are different types of MAC, such as papillary, colloid, signet ring and mixed types (6, 9).
MAC is difficult to diagnose, and when patients are diagnosed, they often already have advanced stage disease (9). Researchers have found that MAC contains a specific genetic abnormality in the AKT1 gene (6).
MAC is a rapidly spreading, aggressive tumour, with a poor long-term outlook. The treatment is surgery to remove the tumour and affected lymph nodes, followed by radiotherapy (9).
Microsecretory adenocarcinoma (MSA)
MSA is a newly identified salivary gland cancer, with only very few reported cases (6, 11). Most cases of MSA occur in the palate or the inner lining of the cheeks, without causing noticeable symptoms (11).
MSA has unique features when examined under the microscope. Tumours contain small tubes and cysts, which leak fluid. The majority of MSA have a genetic abnormality, whereby two genes, MEF2C and SS18 are fused together (6).
MSA is a non-aggressive tumour, and so far, no reported cases have come back or spread to other parts of the body (12). Surgery is the usual treatment (11).
Useful resources
Read more about how to get your tumour profiled and add to the research biobank at the Christie Hospital in Manchester, UK here:
- Gene profiling or tumour profiling or genomic testing - Salivary Gland Cancer UK
- Donate tissue to the Biobank - Salivary Gland Cancer UK
References
- Katabi N, Xu B. Polymorphous Adenocarcinoma. Surg Pathol Clin. 2021;14(1):127-36.
- Sankar Vinod V, Mani V, George A, Sivaprasad KK. Polymorphous low-grade adenocarcinoma-management and reconstruction with temporalis myofacial flap. J Maxillofac Oral Surg. 2013;12(1):105-8.
- Ghannam MG, Singh P. Anatomy, Head and Neck, Salivary Glands. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538325/.
- Weinreb I, Piscuoglio S, Martelotto LG, Waggott D, Ng CK, Perez-Ordonez B, et al. Hotspot activating PRKD1 somatic mutations in polymorphous low-grade adenocarcinomas of the salivary glands. Nat Genet. 2014;46(11):1166-9.
- Xu B, Barbieri AL, Bishop JA, Chiosea SI, Dogan S, Di Palma S, et al. Histologic Classification and Molecular Signature of Polymorphous Adenocarcinoma (PAC) and Cribriform Adenocarcinoma of Salivary Gland (CASG): An International Interobserver Study. Am J Surg Pathol. 2020;44(4):545-52.
- Skálová A, Hyrcza MD, Leivo I. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Salivary Glands. Head Neck Pathol. 2022;16(1):40-53.
- Chen T, Mamdani M, Vescan A, MacMillan C, Davies J. Cribriform adenocarcinoma of the minor salivary glands: a case report. Journal of Medical Case Reports. 2023;17(1):142.
- Sebastiao APM, Xu B, Lozada JR, Pareja F, Geyer FC, Da Cruz Paula A, et al. Histologic spectrum of polymorphous adenocarcinoma of the salivary gland harbor genetic alterations affecting PRKD genes. Mod Pathol. 2020;33(1):65-73.
- Panaccione A, Zhang Y, Mi Y, Mitani Y, Yan G, Prasad ML, et al. Chromosomal abnormalities and molecular landscape of metastasizing mucinous salivary adenocarcinoma. Oral Oncol. 2017;66:38-45.
- Bhat SP, Prasad KH, Bhat VS, Aroor R. Primary mucinous carcinoma of buccal mucosa: a rare case report. Indian J Surg Oncol. 2014;5(3):249-51.
- Bishop JA, Sajed DP, Weinreb I, Dickson BC, Bilodeau EA, Agaimy A, et al. Microsecretory Adenocarcinoma of Salivary Glands: An Expanded Series of 24 Cases. Head Neck Pathol. 2021;15(4):1192-201.
- Panse G. Microsecretory adenocarcinoma: Cutaneous counterpart of a newly described salivary gland tumor with recurrent MEF2C::SS18 fusion. J Cutan Pathol. 2023;50(2):188-90.
Last updated April 2024