Basal Cell Adenocarcinoma (BCAC)
Basal cell adenocarcinoma (BCAC)
Basal cell carcinoma (BCAC) is a rare salivary gland cancer that accounts for 1–3% of salivary gland cancers. BCAC mostly affects people over 50 years of age, with little difference in the number of men and women affected (1, 2). Most BCAC form in the parotid gland (just below and in front of each ear), although there have been some cases of BCAC in the submandibular gland (below the jaws) (2). The parotid gland and submandibular gland are major salivary glands, which are responsible for producing approximately 95% of saliva (3). BCAC forms a slow-growing painless lump, which usually spreads into surrounding nerves and blood vessels (1). Common symptoms include swelling, pain or tenderness, and numbness in the face (2).
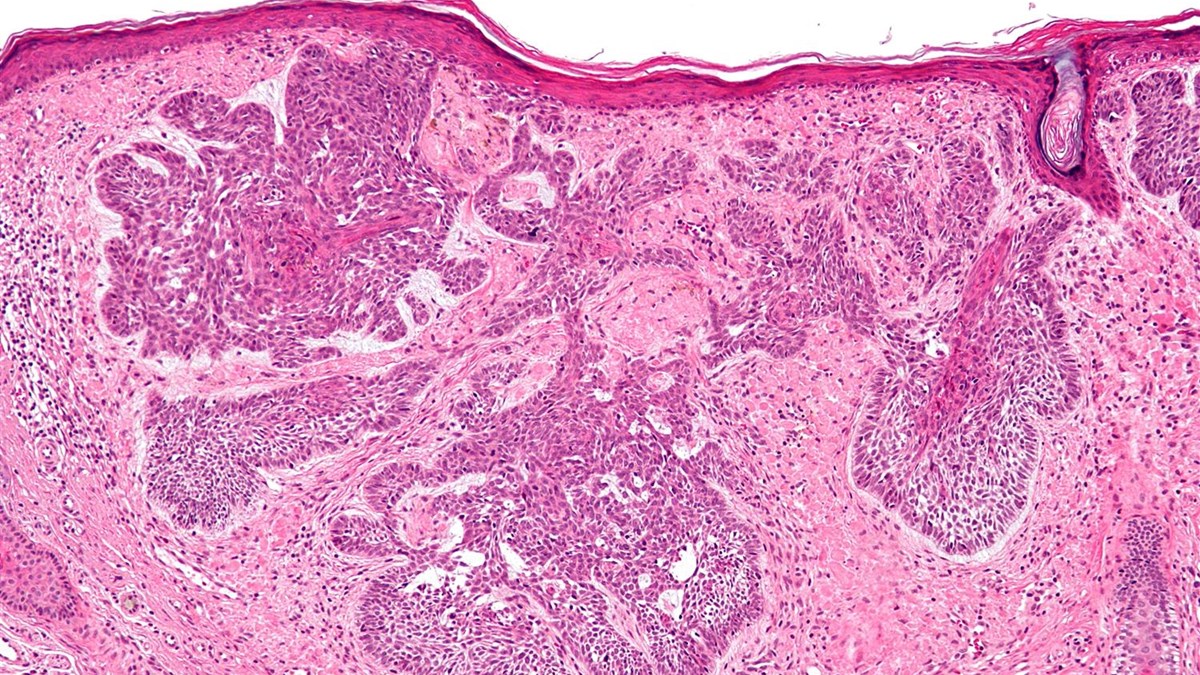
BCAC can be divided into four types based on growth pattern when examined under the microscope: solid, trabecular, tubular, and membranous; of these, the solid type is the most common (4). BCAC is difficult to diagnose as it is very similar to other salivary gland cancers, including basal cell adenoma. BCAC is distinguished from basal cell adenoma by its entanglement with surrounding nerves and blood vessels (1). A combination of methods is used for diagnosis, including biopsy and imaging techniques such as magnetic resonance imaging (MRI) and ultrasound (5).
BCAC is considered a non-aggressive tumour, with a low chance of spreading to other parts of the body. However, tumours have been reported to return in roughly 50% of patients within 10 years (2, 6, 7). The main treatment is surgery to remove the entire cancer, including cervical lymph nodes if the cancer has spread. Radiotherapy is recommended after surgery for patients with late-stage cancer (7).
Useful resources
Read more about how to get your tumour profiled and add to the research biobank at the Christie Hospital in Manchester, UK here:
- Gene profiling or tumour profiling or genomic testing - Salivary Gland Cancer UK
- Donate tissue to the Biobank - Salivary Gland Cancer UK
References
1. Lin H, Huang J, Chen X, Chen X, Hu W. A Rare Case of Basal Cell Adenocarcinoma of the Right Submandibular Gland. Ear Nose Throat J. 2023:1455613231216705.
2. Meyyappan A, Kumar S, Jeyapriya MT, Pradeep S. Basal cell adenocarcinoma-2 case series of a rare entity. Oral Maxillofac Pathol J. 2023;14(1):127-30.
3. Ghannam M, Singh P. Anatomy, Head and Neck, Salivary Glands Treasure Island (FL): StatPearls Publishing; [updated 2023 May 29. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538325/.
4. Ellis GL, Wiscovitch JG. Basal cell adenocarcinomas of the major salivary glands. Oral Surg Oral Med Oral Pathol. 1990;69(4):461-9.
5. Moore MG, Yueh B, Lin DT, Bradford CR, Smith RV, Khariwala SS. Controversies in the Workup and Surgical Management of Parotid Neoplasms. Otolaryngol Head Neck Surg. 2021;164(1):27-36.
6. Thompson L, Wenig BM. Diagnostic Pathology: Head and Neck. 2nd ed: Elsevier; 2016.
7. Pusztaszeri M, Deschler D, Faquin MD P, William C. The 2021 ASCO guideline on the management of salivary gland malignancy endorses FNA biopsy and the risk stratification scheme proposed by the Milan System for Reporting Salivary Gland Cytopathology. Cancer Cytopathology. 2023;131(2):83-9.
Last Updated April 2024