Drug Therapies - Immunotherapy
Understanding the immune landscape in Adenoid Cystic Carcinoma
In immunotherapy the body's own immune system is used to fight cancer by helping it recognize and attack cancer cells.
We talk to Dave Morgan, a post-doc researcher working at the Lydia Becker Institute of Immunology and Inflammation at Manchester University. He tells us more about his research into ACC below.
First things first: What is immunotherapy?
It’s giving a drug that will boost your immune cells response so those cells can target a particular cancer. The advantage of it as a treatment is that immune cells don’t attack your own healthy tissue. That’s the issue with chemotherapy, radiotherapy, and, to an extent, surgical removal; there’s always damage to the patient’s healthy cells, not just the tumour.
Can you explain why research into immunotherapy is needed so urgently in Adenoid Cystic Carcinoma?
OK, so simply defined, Adenoid Cystic Carcinoma is very hard to treat. The only two forms of treatment that are available for it currently are removing it surgically, or radiotherapy. It doesn’t respond to current chemotherapies.
Recently, we’ve been seeing the development of immunotherapies that harness the power of the immune system to kill cancer, but ACC doesn’t respond to any immunotherapies that are currently available. Many of these therapies work by enhancing T cell response. However, Adenoid Cystic Carcinomas don’t have many T cells within the tumour. Very little is known about the immune cells that are based in Adenoid Cystic Carcinomas and other salivary gland cancers.
Where do you begin in developing new immunotherapy treatments for ACC?
The first job is to understand what the immune landscape or environment is within these tumours. This needs to be clearly understood before you can then potentially design drugs with the knowledge you’ve developed. You can just test cocktails of these immunotherapy drugs and see if they work on ACC. But this is very hit and miss. We want to provide the field with information that will enable them to develop new treatments in a more targeted way that reflects the biology of the immune landscape in an ACC tumour. Whether researchers want to chose which existing drugs to trial for ACC, or create completely new treatments, the aim is that our research will allow them to do so in a much more targeted way.
How do you explore the immune landscape in these tumours?
There are two approaches to take in this type of research. Firstly, you can use the part of the tumour that’s removed from a patient during surgery. Secondly, you can get blood that’s taken from the patient – peripheral blood that flows everywhere in the body. In the case of ACC, getting the tumours is pretty rare. That’s because it’s a rare cancer – but also, because of where the tumours are located. They’re generally in the head and neck and around the salivary glands, so getting the primary tumour from there is difficult.
What scientific techniques do you use?
We use a technique called flow cytometry. First, you take a blood sample. You then isolate the white blood cells within that blood by spinning it down in a centrifuge. You get these nice layers, and you can take out the white layer and there will be your immune cells.
Next you want to identify the types of immune cells. To do this we use antibodies – the molecules that bind to specific proteins on the immune cells. By selecting the right combination of antibodies you can identify the immune cells in a sample. The antibodies we use for flow cytometry have fluorescent tags on them. This means that you can put the immune cells tagged with the fluorescent antibodies through a machine, - a flow cytometer - that fires a light at them so they fluoresce. What is special about these antibodies is each one gives off a different colour in the machine, allowing you to identify them, and therefore identify the immune cells in the blood sample.
First we want to look at the broad spectrum of immune cells in these patients, then using what we have learnt, we would then go deeper within these populations of cells to investigate further. For the tumour tissue we do get, you can use the same technique to extract the immune cells, but first you can free the individual cells from the tumour sample. We achieve this by using scissors to chop the tumour into little pieces, enzymes to break down the samples even further and then very fine sieves to clear away the debris, leaving you with live cells. Another method of investigating the tumour sample is to look at really, really thin slivers of the tumour under the microscope, again using fluorescently tagged antibodies.
What’s the best material for your research?
The tumour is the ideal material because that is where you’d want the drugs to target – it’s where the immunotherapy would be acting. It’s all about understanding why the current immunotherapies aren’t working on these tumours. But you can get lots of information from the blood changes, too.
How does the SGC Biobank in Manchester help your research?
When a tumour is removed, the surgeon will take a sample to be sent to the pathologist so the tumour can be profiled and the patient can understand exactly what type of cancer they have. But there’s usually leftover tumour, which can then be put in wax to preserve it. If this is then donated for research by a patient to our Salivary Gland Cancer Biobank, we can use it to understand these cancers better.
How has COVID-19 affected your research?
I began this project in January 2020. At the beginning, we were banking as many blood samples as we could until we had enough to begin work. Then Coronavirus came and subsequently, everything’s been delayed. But now, in September, the University is opening up again, and samples are starting to come back in.
We may have to change our approach a bit – as before COVID hit, patients with Adenoid Cystic Carcinoma were coming into a clinic in Manchester from all across the country, and that’s how we were getting the blood samples. However, now these clinics are being done mainly over the phone, so we’re limited to a base of Manchester patients, which is a small number of people. So what we’ll be doing is also collecting samples from patients with other head and neck cancers that are less rare, but do respond to immunotherapy. We can analyse these samples, and then, when we get more ACC samples in again, we will be able to compare the two. Comparing responding samples from other head and neck cancers, and the non-responding ACC samples will help us to hone in on why current immunotherapies don’t work in ACC.
How are new technological developments helping your research?
The main challenge in ACC research of this type is the rarity of the physical tumour and the size of it – because they tend to be pretty small. It’s limiting, both in terms of how often you get new tissue, and the number of cells in each sample. But there are new technologies developing that would allow us to make better use of these tumours. There are now evolved versions of flow cytometry and microscopy, called mass cytometry and imaging mass cytometry. Instead of tagging the antibodies with fluorescent markers and identifying them according to the colour of light they give off, it works by labeling them with heavy metal ion tags.
This is useful as in the fluorescence spectrum, which is like the rainbow of light, you’ve only got so many colours, and certain colours overlap with each other. This means you’re limited as to the number of antibody tags you can use at a time – normally around 10 for flow cytometry and 3-4 for microscopy. Having metal tags means you can tag many more antibodies, around 30, and each one has a nice, clean signal. The major advantage this has is being able to get a lot more information out of a limited amount of sample, which when researching a disease like ACC is incredibly valuable.
Are you involved in the work to create mouse models for ACC?
I’m not, no, but here in Manchester they are working to generate mice that would develop this brand of tumour. It’s early days in that work. They have to do the gene editing to create these mice so it can take years. These exist already in the US, but we want to generate a different version here in the UK. They are created to get an understanding of how the cancer works within the whole system of an animal, and to understand the biology of the tumour and its progression. In humans, these tumours grow very slowly, and they’re small, so you often don’t notice it early on. But in a mouse model, you can watch it develop right from the beginning. Later down the line, they could also be used to test the effectiveness of drugs in stopping the growth of ACC tumours.
Why did you choose to research into ACC?
On a scientific level, it’s a very interesting thing to work on, as there’s not much known about it. That means I will be one of the first people to be exploring the immunological landscape of ACC tumours directly, which is really exciting. It’s also great to think that this research might directly benefit patients. Hopefully, we will make discoveries that allow us to really understand what’s going on in an ACC tumour, which will aid everybody down the line in creating improved treatments. And that is what we all hope for in an area such as immunology – that our work will have an impact in the clinic. Even if it’s not us directly designing the drugs – we’re helping provide the understanding which will aid others to develop treatments. It’s also exciting to be using new scientific techniques, and to make the most of very rare and precious samples.

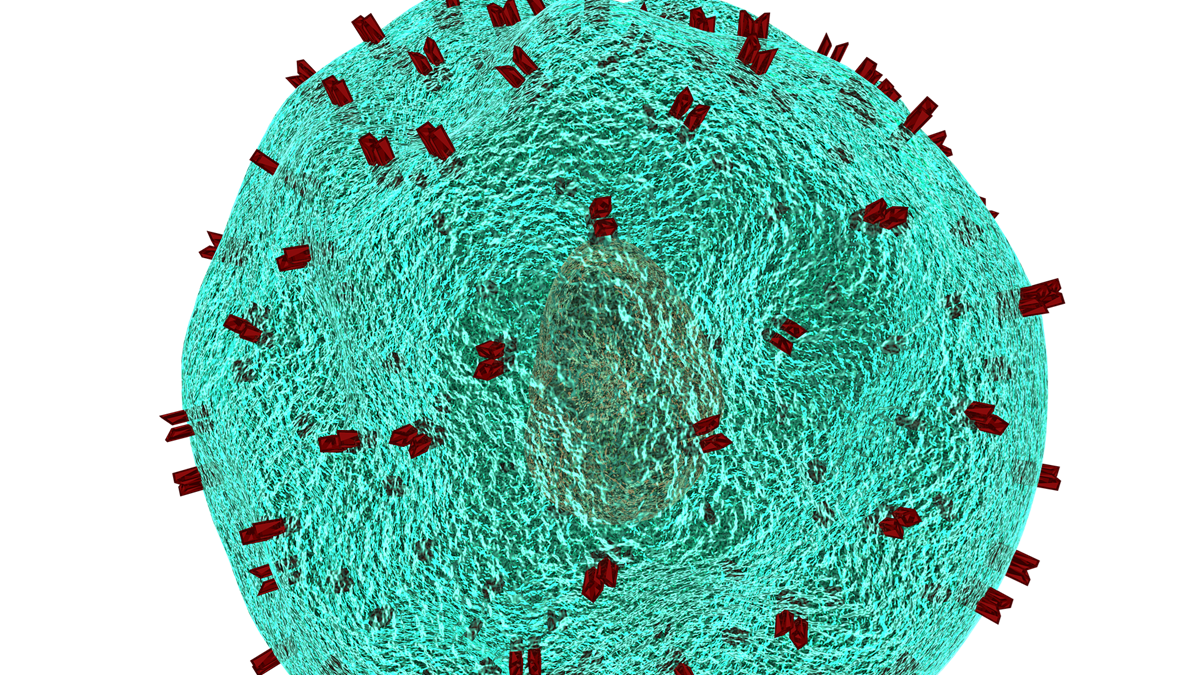 Image credit: Image by allinonemovie at Pixabaya
Image credit: Image by allinonemovie at Pixabaya